The fast-paced digital age offers numerous solutions to streamline AR management. Medical billing software, for instance, can automate many aspects of the billing process, reducing the chance of human error and accelerating the payment cycle. Your staff should start to work from the largest accounts first when making the collection calls to patients. Medical billing software can streamline your entire collections process by tracking various things simultaneously such as past-due bills, identifying those patients who have fallen behind, and automating late fees. However, this software might be costly but one needs to understand that the software will end up saving a lot on internal billing resources as well as increase your collection rate.
A Step-by-Step Guide to Managing Your A/R for Maximum Cash Flow
This option generally has the most effective accounts receivable collection rates because your system has defined them as the most likely to collect. Creating consistent, clear communications is the surest way to keep your AR department running smoothly and ensure that money’s coming in. Sending out payment reminders, post-due notices, formal dunning letters, and legal notices is a vital function of your AR team. Maintaining the appropriate language and tone in each of these communications can make a major difference in receiving payments on time. The subsequent sections of this guide delve into how AR applies specifically to medical practices, common AR challenges faced, and how to overcome them. Consequently, high AR can lead to cash flow problems, impacting the practice’s ability to cover operational expenses, invest in new equipment or training, and ultimately provide the best possible patient care.

Strategies for Prioritizing Patient Accounts Receivable

The front office worker should ask for communication updates on the policyholders, policy IDs, preferred communications, and patient portal access before check-in processes. Check-in and collecting outstanding bills at the front desk before being seen give the patient and the physician a strong and trusting start. Therefore, hiring an effective medical billing professional who specializes in A/R follow-ups will assure that your practice, clinic, or a larger healthcare facility is successful and equipped to treat more people. One of the main sources of revenue for a medical institution, such as a hospital, is the account receivable payments they get either from the patient or their insurance company.

How do patient payments impact A/R management?
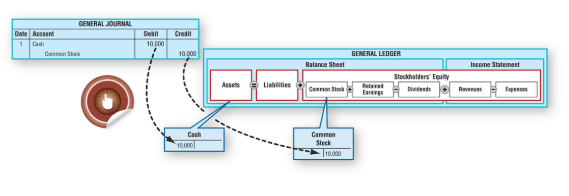
AR helps ensure positive cash flow, fewer claim denials, and improved regulatory compliance. In medical billing, anything that makes a patient feel more empowered and in control is a plus. What is bookkeeping By evaluating real-time data with deep visibility, a healthcare organization can also more easily identify potential issues and slowdowns in their system. A strong business is built on an excellent customer experience—one that’s as transparent and supportive as possible. A healthy AR process can make it easier to circumvent and ameliorate issues like insurance claim denials, freeing up time to focus on stronger relationships and better patient care.. Accounts receivable management, though often challenging, is an integral aspect of the financial health of any medical practice.
- Whether your patients and customers prefer physical invoices, digital transactions, email attachments, or other forms of communication, an automated system makes sure you stay connected.
- Medical Billers and Coders (MBC) has been providing account receivable services to clients across the USA.
- Learn the average of your Medicaid turnaround to know if their payment response is good.
- Your billing staff should perform insurance eligibility verification before the date of service to avoid this patient responsibility enters into AR cumulation.
- ZOLL Data Systems teams up with industry innovators to leverage and enhance data-driven solutions that deliver maximum value to our customers.
- Clearly, outdated workflows and operations end up costing a healthcare organization more than upgrading to a modern, automated solution.
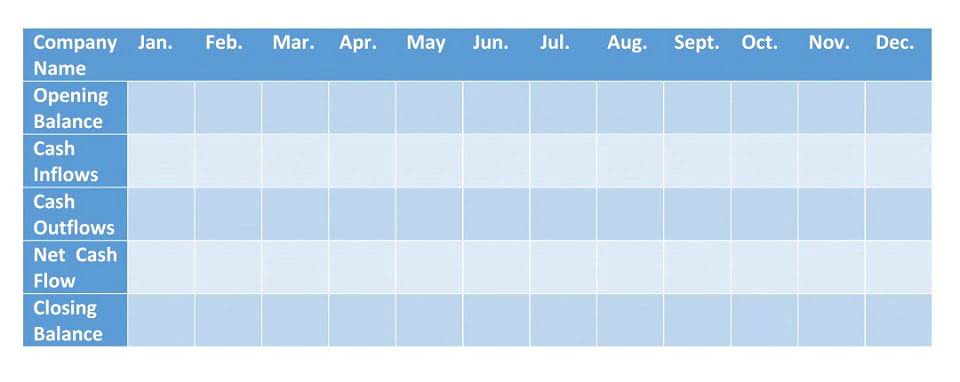
Displays the last payment made by the responsible party (insurance or patient). Claims submitted within the last days based on the defined filter setting on the “Show Aging by” and the defined aging reference date (“As of”). Enter up to five patients to filter the report to only include the targeted patients. Enter up to five insurance plans to filter the report to only include the accounts receivable log for individual patients targeted plans. When prepping to make a transition into a new workflow model, you’ll want to do some “spring cleaning” first. We recommend employing a few tactics to help you quickly clean up accounts receivable components, and to avoid bringing dormant, non-collectable accounts into the new work flow model.
Specialty and Service Society
- Reasons include some patients viewing aging on the statement as “more time to pay” and credit may confuse the patient.
- But manual, outdated collection processes (e.g. spreadsheets, disparate systems and tools, paper forms, etc.) can make it difficult to capture and update customer information.
- By comprehending and effectively managing Accounts Receivable, medical practices can improve their financial health, ensuring they have the necessary resources to continue providing exceptional patient care.
- This enables AR offices to send out reminders, when necessary, and stay on top of customers who are becoming potential credit risks.
This functionality provides pharmacies with a range of benefits and capabilities to enhance their operations and improve customer satisfaction. Medical organizations generate high volumes of documents involving complex data. Using an automated system driven by rules makes it easy to scale production to meet your Opening Entry changing needs. Documents and content can be easily customized for more effective communications with different audiences, and even individual patients and customers.